How I Found My Rhythm After Baby — A Real Postpartum Comeback
After having my baby, everything felt off—my body, energy, even my sense of self. I didn’t realize how much postpartum life reshapes your rhythm until I learned to rebuild it. This isn’t about quick fixes, but real, sustainable healing. With professional guidance and small daily choices, I found balance. If you're feeling lost in the haze of motherhood, this journey might just resonate—and help you reclaim your flow too.
The Hidden Struggle of Postpartum Life
Childbirth is often celebrated as a joyful milestone, but what follows can be far more complex than society acknowledges. Many women enter the postpartum period expecting only happiness, only to be met with overwhelming fatigue, unpredictable emotions, and a sense of disconnection from their former selves. These experiences are not signs of weakness—they are common, biologically rooted responses to one of life’s most profound transitions. The postpartum phase is not simply a recovery from delivery; it is a full recalibration of the body, mind, and daily existence.
Physically, the body undergoes dramatic shifts. Hormone levels that soared during pregnancy plummet within days after birth, particularly estrogen and progesterone. This sudden drop can affect mood regulation, sleep quality, and energy levels. It’s no surprise that many new mothers report feeling emotionally raw or unusually tearful in the first weeks. These symptoms, often referred to as the “baby blues,” affect up to 80% of women and typically resolve within two weeks. However, when these feelings persist or intensify, they may signal postpartum depression or anxiety—conditions that require professional attention.
Beyond hormones, the physical toll of childbirth itself cannot be underestimated. Whether the delivery was vaginal or cesarean, the body has endured significant strain. Tissues need time to heal, muscles must regain strength, and internal systems—such as digestion, circulation, and core stability—must reestablish balance. Yet, societal expectations often pressure new mothers to “bounce back” quickly, ignoring the reality that true healing takes months, not weeks.
Equally impactful is the shift in identity. For many women, becoming a mother reshapes their sense of purpose, priorities, and self-worth. The routines that once defined their days—work, hobbies, socializing—are replaced by feeding schedules, diaper changes, and constant vigilance. This loss of personal rhythm can lead to feelings of isolation or invisibility. The woman who once felt in control may now feel like she’s merely reacting to her baby’s needs, with little space for her own.
Understanding these challenges is the first step toward healing. When a new mother recognizes that her fatigue, mood swings, or sense of disorientation are not personal failings but natural responses to a life-altering event, she can begin to treat herself with compassion. The postpartum period is not about returning to normal—it’s about building a new normal, one that honors both the demands of motherhood and the needs of the self.
What “Life Rhythm” Really Means for New Mothers
Life rhythm refers to the internal and external patterns that govern our days—when we sleep, eat, move, and connect with others. These rhythms are deeply tied to our circadian biology, hormonal cycles, and emotional well-being. Before motherhood, many women operate on a relatively predictable schedule: waking at a consistent time, eating meals at regular intervals, exercising, working, and winding down in the evening. But after childbirth, these rhythms are disrupted, often in ways that feel chaotic and unmanageable.
The most immediate disruption is to the sleep-wake cycle. Newborns feed every two to three hours, day and night, fragmenting what was once a consolidated eight-hour sleep block into short, unpredictable bursts. This chronic sleep disruption affects more than just energy levels—it impairs cognitive function, emotional regulation, and immune response. Studies show that sleep deprivation in the postpartum period is strongly linked to increased risk of mood disorders, reduced milk supply, and slower physical recovery.
Meal timing is another rhythm that often falls apart. With the constant demands of feeding and caring for a baby, many new mothers skip meals, eat on the go, or rely on convenience foods. Irregular eating patterns can lead to blood sugar fluctuations, which in turn affect energy, mood, and concentration. When the body lacks consistent nourishment, it becomes harder to manage stress and maintain emotional stability.
Movement is also deeply affected. Before birth, a woman may have had a regular exercise routine, whether it was walking, yoga, or strength training. After delivery, physical activity often stops entirely, not out of choice but necessity. The body needs time to heal, and many women are unsure when—or how—it’s safe to resume movement. This sudden inactivity can lead to stiffness, weakness, and a sense of physical disconnection.
Emotional rhythm, too, is thrown off balance. The constant caregiving role can leave little room for self-reflection, conversation, or emotional processing. Many women report feeling emotionally “flat” or overwhelmed, unable to access the range of feelings they once had. Without intentional moments of connection—whether through talking with a partner, journaling, or simply pausing to breathe—the emotional system becomes dysregulated.
Rebuilding life rhythm is not about imposing rigid schedules, but about creating gentle, consistent patterns that support healing. It means aligning with the baby’s natural cycles while also carving out small moments for self-care. It means eating at regular intervals, even if meals are simple. It means moving the body in ways that feel safe and restorative. And it means making space for emotional expression, whether through conversation, writing, or quiet reflection. Over time, these small acts of consistency help the body and mind reestablish a sense of order and calm.
Why Professional Support Is Non-Negotiable
In the early weeks after childbirth, new mothers are often surrounded by advice—from family, friends, online communities, and even strangers. While much of this guidance comes from a place of care, not all of it is accurate or safe. Some suggestions may be outdated, others overly restrictive, and a few could even be harmful. This is why professional medical support is essential during the postpartum period. Healthcare providers such as obstetricians, midwives, pelvic floor therapists, and mental health specialists offer evidence-based guidance tailored to individual needs.
One of the most important aspects of professional care is the postpartum checkup, typically scheduled around six weeks after delivery. This appointment is not just a formality—it’s a critical opportunity to assess physical healing, screen for complications, and discuss emotional well-being. During this visit, a healthcare provider can evaluate the recovery of the perineal area, check for signs of diastasis recti (abdominal separation), and assess pelvic floor function. They can also review any ongoing symptoms, such as pain, urinary incontinence, or bleeding, and recommend appropriate interventions.
Pelvic floor therapy, in particular, is a valuable resource that many women overlook. The pelvic floor muscles support the bladder, uterus, and rectum, and they undergo significant stress during pregnancy and childbirth. Weakness or dysfunction in this area can lead to issues like urinary leakage, pelvic pain, or discomfort during intercourse. A pelvic floor physical therapist can guide a woman through targeted exercises and manual techniques to restore strength and coordination, often preventing long-term problems.
Mental health support is equally crucial. While the “baby blues” are common and usually temporary, postpartum depression and anxiety affect approximately 1 in 7 women and can have serious consequences if left untreated. Symptoms may include persistent sadness, excessive worry, difficulty bonding with the baby, or thoughts of self-harm. A mental health professional can provide therapy, support groups, or, if needed, medication to help manage these conditions. Early intervention makes a significant difference in recovery outcomes.
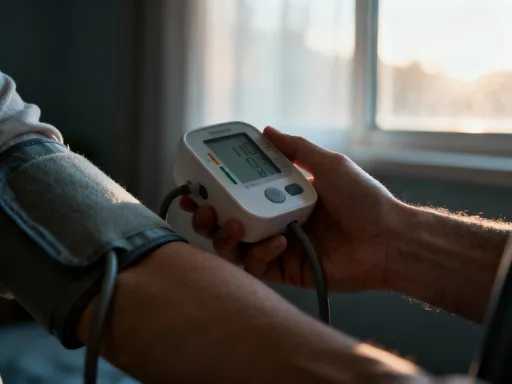
Professional support also helps women navigate the overwhelming amount of information available today. From conflicting feeding advice to conflicting exercise guidelines, it’s easy to feel confused or anxious. A trusted healthcare provider can clarify what is safe, effective, and appropriate for each individual. They can help a woman distinguish between normal postpartum changes and signs that require further evaluation, such as high blood pressure, signs of infection, or blood clots.
Seeking professional care is not a sign of failure—it’s an act of responsibility and self-respect. It acknowledges that healing from childbirth is a medical process, not just an emotional one. By working with qualified experts, new mothers can recover more safely, confidently, and completely.
Rebuilding Your Body’s Clock: Sleep and Energy Management
Sleep disruption is one of the most universal and challenging aspects of early motherhood. Unlike other forms of fatigue, postpartum sleep deprivation is not just about quantity—it’s about fragmentation. Instead of cycling through deep and restorative sleep stages, new mothers often experience brief, interrupted periods of light sleep, which do little to restore energy or cognitive function. Over time, this can lead to mental fog, irritability, and reduced resilience to stress.
The key to managing energy in this phase is not to aim for perfect sleep—but to work with the reality of the situation. One effective strategy is to align with the baby’s natural sleep cycles. Since newborns tend to sleep in short bursts, mothers can use those same windows to rest. Even 20 to 30 minutes of closed-eye rest can help reset the nervous system and improve alertness. The goal is not to “get things done” during these breaks, but to allow the body and mind to recover.
Another important factor is light exposure. Natural daylight helps regulate the body’s internal clock, or circadian rhythm. When possible, spending time near a window or stepping outside during daylight hours—especially in the morning—can help reinforce the distinction between day and night. This makes it easier to stay alert during waking hours and more likely to feel sleepy at night. Conversely, minimizing bright lights and screen exposure in the evening supports the production of melatonin, the hormone that promotes sleep.
Creating a restful environment also makes a difference. A quiet, dimly lit space with minimal distractions can make micro-rests more effective. Using white noise machines or earplugs can help block out sudden sounds. If a partner or support person is available, coordinating care responsibilities can allow for longer stretches of uninterrupted rest, even if only once every few days.
Nutrition and hydration also play a role in energy management. Skipping meals or drinking too much caffeine can lead to energy crashes and worsen sleep quality. Eating balanced snacks that include protein, healthy fats, and complex carbohydrates helps maintain steady blood sugar levels, which supports sustained energy. Drinking water throughout the day prevents dehydration, which can mimic or worsen fatigue.
Finally, it’s important to let go of the idea that productivity must equal value. In the postpartum period, rest is not laziness—it is active healing. Every moment of stillness allows the body to repair tissues, regulate hormones, and rebuild strength. By reframing rest as a necessary and powerful act of recovery, mothers can reduce guilt and embrace the pace that their bodies need.
Nourishment That Supports Healing and Balance
Nutrition in the postpartum period goes far beyond general “eating healthy.” It is a form of medicine—a way to support tissue repair, hormone regulation, milk production (if breastfeeding), and emotional stability. The body has just completed a physically demanding process, and it needs consistent, high-quality fuel to recover. Yet, many new mothers struggle to prioritize meals amid the constant demands of infant care.
One of the most important goals is to stabilize blood sugar. When meals are skipped or consist mostly of refined carbohydrates, blood sugar levels spike and crash, leading to fatigue, mood swings, and cravings. Eating small, frequent meals every three to four hours helps maintain steady energy. Each meal should ideally include a source of protein (such as eggs, chicken, beans, or Greek yogurt), healthy fats (like avocado, nuts, or olive oil), and fiber-rich carbohydrates (such as whole grains, vegetables, or fruit). This combination slows digestion and prevents sharp fluctuations in blood sugar.
Hydration is equally critical. Breastfeeding mothers, in particular, need additional fluids to support milk production. Dehydration can lead to headaches, constipation, and reduced energy. A simple way to monitor hydration is by checking urine color—pale yellow indicates adequate fluid intake. Keeping a water bottle nearby and sipping throughout the day makes it easier to meet this need without having to remember large amounts at once.
Certain nutrients play specific roles in postpartum recovery. Iron is essential, especially if there was significant blood loss during delivery. Low iron levels can contribute to fatigue and weakness. Good dietary sources include lean red meat, lentils, spinach, and fortified cereals. Vitamin C, found in citrus fruits and bell peppers, enhances iron absorption. Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, support brain health and may help reduce the risk of mood imbalances.
Planning simple, nourishing meals in advance can reduce daily stress. Preparing freezer-friendly dishes like soups, stews, or casseroles before the baby arrives—or accepting meal deliveries from friends and family—ensures that healthy options are always available. Even basic combinations, like toast with peanut butter and banana, or oatmeal with nuts and fruit, provide balanced nutrition without requiring much effort.
It’s also important to avoid restrictive diets during this time. The postpartum body is not a project to be fixed—it is a system in recovery. Fad diets, extreme calorie restriction, or elimination of entire food groups can delay healing and increase the risk of nutrient deficiencies. The focus should be on abundance, not deprivation. Eating enough calories—especially if breastfeeding—supports milk supply, energy levels, and emotional well-being.
Over time, as energy returns and routines stabilize, women can gradually reintroduce more variety into their diets. But in the early months, the priority is consistency, balance, and ease. Nourishment is not about perfection—it’s about showing the body kindness through food.
Movement as Medicine: Gentle Steps Back to Strength
Movement after childbirth should not be approached as a return to fitness, but as a return to connection—with the body, breath, and self. Too often, women feel pressure to resume intense exercise soon after delivery, only to experience pain, setbacks, or discouragement. The truth is that the body needs time to heal, and the right kind of movement at the right time can accelerate recovery, while the wrong kind can cause harm.
The first phase of postpartum movement should focus on awareness, not exertion. Simple practices like diaphragmatic breathing help reestablish the mind-body connection and support core function. Lying on the back with one hand on the chest and one on the belly, a woman can practice slow, deep breaths that expand the lower ribs and engage the diaphragm. This not only calms the nervous system but also gently activates the deep core muscles that were stretched during pregnancy.
Pelvic floor awareness is another foundational practice. Many women are unaware of how to properly engage these muscles. A gentle contraction—like stopping the flow of urine—can be practiced while lying down, sitting, or standing. These exercises, often called Kegels, help restore tone and control. However, it’s important to ensure that the muscles are not overly tight or compensating, which is why guidance from a pelvic floor therapist can be invaluable.
Once basic awareness is established, gentle walking can be introduced. A short stroll around the neighborhood, even just five to ten minutes at first, promotes circulation, supports mood, and encourages mobility without strain. As strength and endurance improve, walks can gradually increase in duration and pace. The key is to listen to the body—pain, heaviness, or leaking urine are signs to slow down or rest.
Core retraining comes later, typically after six to eight weeks and with medical clearance. Exercises like heel slides, pelvic tilts, and gentle abdominal bracing help rebuild stability without putting pressure on healing tissues. Movements that involve crunching, twisting, or heavy lifting should be avoided until the core is fully reconnected and any diastasis recti has improved.
The goal of postpartum movement is not to burn calories or lose weight, but to restore function, confidence, and body trust. Each small step—whether it’s a deep breath, a mindful contraction, or a short walk—contributes to long-term strength and well-being.
Creating Emotional Rhythm: Connection, Boundaries, and Self-Compassion
Emotional well-being in the postpartum period is not about avoiding difficult feelings, but about creating space to experience and process them. Hormonal shifts, sleep deprivation, and the intensity of newborn care can lead to mood swings, irritability, and moments of overwhelm. These reactions are normal, but they can feel isolating without intentional emotional support.
One of the most powerful tools for emotional regulation is connection. Talking with a trusted friend, partner, or counselor allows a woman to express her fears, frustrations, and joys without judgment. Even brief conversations can help release emotional tension and provide perspective. Journaling is another effective outlet—writing down thoughts, feelings, or simple observations helps organize the mind and create clarity.
Equally important is setting boundaries. Well-meaning visitors, advice, and social expectations can add pressure during a time when rest and privacy are needed. It’s okay to say no to visitors, delay social events, or ask for help with household tasks. Protecting time and energy is not selfish—it’s necessary for healing. Simple strategies, like scheduling visits, limiting time with guests, or designating a “no talk” hour each day, can help maintain emotional balance.
Self-compassion is perhaps the most transformative practice. Many new mothers hold themselves to impossibly high standards, believing they should be able to do it all—care for the baby, manage the home, and feel joyful all the time. When reality falls short, guilt and shame can follow. Replacing self-criticism with kindness—acknowledging effort, honoring limits, and recognizing progress—shifts the emotional landscape. Phrases like “I’m doing my best” or “This is hard, and that’s okay” can be powerful reminders of self-worth.
Over time, these small emotional habits—talking, writing, setting limits, being kind—create a rhythm of stability. They don’t eliminate challenges, but they build resilience. Emotional healing, like physical healing, is not linear. It moves in waves, with good days and difficult ones. But with consistent care, the overall trajectory moves toward balance, strength, and peace.
Conclusion
Postpartum recovery isn’t a race—it’s a reweaving of body, mind, and time. By honoring your natural rhythm and seeking professional support, you build a foundation that lasts far beyond the first year. This journey isn’t about returning to who you were, but becoming who you are now: stronger, wiser, and deeply in tune. The challenges of early motherhood are real, but so is the capacity to heal, adapt, and thrive. With patience, care, and the right support, every woman can find her rhythm again.